Day 16 :
- Cornea and Refractive Surgery | Cataract Surgery | Eye Diseases | Glaucoma | Contact Lens
Location: Paris

Chair
Kenneth Seger
Nova Southeastern University College of Optometry, USA
Session Introduction
Kenneth Seger
Nova Southeastern University College of Optometry, USA
Title: Lower order aberrations and contact lenses: A rationale for 0.50DC toric soft lenses

Biography:
Dr. Kenneth R. Seger has been on the faculty at Nova Southeastern University College of Optometry for 18 years. Prior to that he spent six years in private practice in his hometown, San Luis Obispo, CA followed by 16 years as part-time clinical faculty at the University of California Berkeley School of Optometry.
At NSUCO Dr. Seger has pursued research interests in contact lenses, myopia development and (with Dr. Ava Bittner) a unique treatment modality for RP.
Abstract:
PURPOSE: Lower order aberrations have been correctable for generations; defocus for hundreds of years and an astigmatism for over a century. For the last several years there has been considerable interest in correcting higher order aberrations (HOA). However, as of now, toric soft lenses, which have become so reliable that they are manufactured as daily disposables, have 0.75DC as their lowest cylindrical correction. This leaves many patients with an uncorrected cylindrical component which causes a greater negative impact of vision than typical uncorrected HOA values. Is there a need or justification for manufacturing -0.50DC toric lenses?
METHODS: The data of all spectacle lens prescriptions for three consecutive months was obtained from an independent spectacle lens fabrication laboratory. The cylindrical component powers were tabulated and analyzed. The number of current toric lens combinations and additional lens combinations necessary for 0.50DC correction was calculated.
RESULTS: Out of 3869 consecutive spectacle lens prescriptions 778 (20.1%) had correction of -0.50DC (27.3% of all cylindrical corrections), suggesting that 20% of potential lens wearers have significant residual astigmatism. Using the parameters of sphere power of +6.00 to -8.00 (in 0.25D steps) with cylindrical corrections of 0.75, 1.25, 1.75 and 2.25 DC in round the clock axis steps of every 10 degrees 3816 lens alternatives need to be available. To incorporate -0.50DC correction an additional 934 lens parameters (an increase of 24.5%) would be necessary.
CONCLUSIONS: Increasing the toric lens inventory by ~25% would theoretically capture an additional 20% of currently less-than-optimally corrected potential contact lens wearers. We suggest contact lens manufacturers, in addition to pursuing HOA correction, might more profitably work on developing a 0.50DC toric lens.
Zamora-Ortiz Rocio
Military Hospital, Mexico
Title: Histopathological findings in secondary corneal refractive surgery ectasias
Biography:
Rocío Zamora is a surgeon ophthalmologist with a fellowship in Microsurgery of Anterior Segment of the Eye and a fellowship in Córnea and Refractive Surgery. Nowdays she is working in Mexican institutes as Military Hospital and in private practice.
Abstract:
ABSTRACT
Introduction
Corneal ectasia is one of the most serious complications after refractive surgery and although some risk factors are known, mechanisms ectasia post refractive surgery are not entirely clear.
Material and Methods
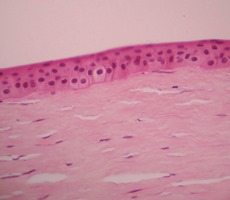
Retrospective, observational, cross-sectional, descriptive study. Histopathological reports and slides of patients with ectasia secondary refractive surgery treated with penetrating keratoplasty were reviewed. Microscopic to measure corneal thickness and describe changes in the corneal layers pictures were taken.
Results
The average corneal thickness greater area ectasia was 344.83 microns and the average was 38.06 microns epithelium. In LASIK cases, the average thickness of the flap and was 162.29 microns 181.34 microns residual stromal bed. The most frequent alterations were atrophy and epithelial hyperplasia (62%), partial loss of Bowman layer (42%) and endothelial (56%) decrease. (Photomicrograph 1).
Discussion
Alterations in subsequent layers of the cornea as a decrease in the stromal bed and endothelial loss, are risk factors for corneal ectasia, which we support with our results; we add alterations in the previous layers.
Conclusions
The findings of the previous layers of the cornea are histopathological factors that may contribute to the formation of corneal ectasia.
Shroug M Aldaham
Ministry of Education, Saudi Arabia
Title: Mesopic visual function is not equally impaired in type 2 diabetics without retinopathy

Biography:
Shroug Aldaham has recently graduated from Complutense University of Madrid (UCM), Spain with a PhD degree in Optics, Optometry and Vision. She has a BSc (Hons) in Optometry from King Saud University (KSU), Riyadh, Saudi Arabia, and a Master of Science in Vision Science from the University of Waterloo, Ontario, Canada. She has joined the Optometry department at KSU as a demonstrator (an academic position that prepares for professorship) before joining the Master program in Canada. After her masters she returned to Riyadh and later joined the PhD program at UCM. Both of her Masters and PhD studies were Saudi government-funded research grants. She has a research experience in pediatric vision screening and visual function testing in diabetics and has published in international optometric and vision research meetings. Her research interests are pediatric and diabetic visual function.
Abstract:
Background: Early retinal neurosensory dysfunction occurs before any apparent retinal vascular changes in type 2 diabetes.(1,2) It has been reported that diabetics without retinopathy show a decrease in mesopic letter contrast sensitivity(2) and in low contrast visual acuity..(3-5) The information however is lacking about whether different visual tests would show equal mesopic visual dysfunction or not. Purpose: The purpose of this study therefore is to assess mesopic visual function in type 2 diabetics without retinopathy, with well controlled glucose level, and compare it with healthy controls using three visual tests. Methods: This cross-sectional study included thirty-four normal controls and thirty type 2 diabetics without retinopathy, with age and sex matched and well controlled glucose level. Three visual function tests were assessed under mesopic luminance conditions (high and low contrast visual acuity, contrast sensitivity using sinusoidal gratings at low spatial frequencies of 0.5, 1, and 2 cycles per degree, and disk halo size). Results: Type 2 diabetics showed a worse high and low contrast visual acuity and a larger disk halo size compared to healthy subjects, but did not show any change in contrast sensitivity at low spatial frequencies. Conclusions: Type 2 diabetics without retinopathy do not show equal mesopic visual dysfunction for the three visual function tests.
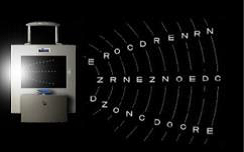
This presentation will further examine the visual tests’ differences aiming to see which test can be used as a screening tool for diabetics to detect early visual changes before the onset of retinopathy.

Biography:
Kumale Tolesa has completed Doctor of Medicine degree from Jimma University, School of Medicine and Ophthalmology specialty. She is an Assistant
Professor of Ophthalmology in Jimma University. She has published 4 papers in reputed journals and has 6 more pending publications. She has inclination towards
Glaucoma and Pediatric Ophthalmology. She did a short term fellowship on Pediatric Ophthalmology and strabismus at Gachon University Gil Hospital, South
Korea and Tilganga Institute of Ophthalmology, Nepal.
Abstract:
Glaucoma is the second leading cause of blindness worldwide, accounting for 15% of blindness. According to WHO estimate,
people with high Intraocular pressure (IOP), >21 mm Hg, are around 104.5 million. People who are blind due to glaucoma
are estimated to be 8 million. To date glaucoma community screening is a point of controversy. The aim of this study was to
determine the proportion of glaucoma among adults aged 40 years and above who had participated on a community screening
program in Jimma University, Department of Ophthalmology. A cross-sectional study was conducted among volunteer
residents of Jimma town and surrounding area with age 40 years and above who came on a community screening program
conducted after media announcement. The participants were interviewed by trained data collectors and complete ophthalmic
examination was performed in all cases by general ophthalmologists or/and glaucoma specialist. The data was analyzed using
SPSS for Windows version 16.0 software. X2 test was performed and P-value<0.05 was considered significant. Of the adults
who came for the screening, 47 (10.24%) were diagnosed to have glaucoma, 59 (12.85%) were glaucoma suspects, and 8
(1.74%) had ocular hypertension. The prevalence of primary open angle glaucoma (POAG) was the highest (42.55% of all new
glaucoma cases, and 4.4% of all screened adults). Around 5.7% of all glaucoma cases were found to be blind. Female sex, lower
level of education, high blood pressure, and higher intraocular pressure were associated with glaucoma (P- value<0.05, 99%
CI). Female sex and younger age group were associated with POAG, whereas older age was associated with Pseudoexfoliative
glaucoma (P-value<0.05, 99% CI). Glaucoma awareness creation and glaucoma community screening should be promoted for
early diagnosis and intervention to prevent irreversible blindness.
Serge Picaud
Institut de la vision, France
Title: Visual restoration by retinal prostheses and optogenetic therapy : Validation in nonhuman primates.

Biography:
Serge Picaud director for Institut de la Vision, Team Leader - Retinal information processing: Pharmacology,toxicology, pathologies. Founder in Fovea Pharmaceuticals,
Founder in Pixium Vision, member of the scientific committee for the Federation des Aveugles de France, member of the administrative committee for the Fondation Voir
et Entendre, member of the CNRS committee for the section 25, member of ANR funding committee, member of AERES Committee
Abstract:
Following photoreceptor loss, electrical activation of residual retinal neurons can restore some visual function in blind
patients. However, the perception provided by current devices does not allow face recognition or autonomous motion
in an unknown environment. At the Vision Institute in Paris, we have assessed new photovoltaic retinal implants and
optogenetic therapy on non-human primates to improve further current strategies for restoring vision. Using photovoltaic
implants, individual retinal ganglion cells were activated by infrared activation of a single 100μm pixel and not by its neighbors
indicating thereby high resolution of the device. In vivo, photoreceptors were found to degenerate below the implant due to
the retinal detachment from the retinal pigment epithelium. Behavioral studies confirmed the presence of a blind spot upon
normal visual stimulation at the implant position. However, infrared stimulations at the implant position induced saccades
indicating thereby visual perception generated by the infrared sensitive implants. In parallel, microbial opsins were expressed
in the non-human primate retina through gene therapy. Activation of the retinal ganglion cells with patterns and short pulse
durations (1-10 ms) demonstrated the potential use of this strategy for visual restoration up to 6 months post injection. These
new results demonstrate efficacy on non-human primates for both photovoltaic implants and optogenetic therapy paving their
ways towards clinical trials.
- Pediatric Optometry | Clinical Optometry | Neuro Optometry | Myopia
Location: Paris

Chair
Nuha Fath Elrahman
Al-neelain University college of Optometry and Visual science, Sudan
Session Introduction
Hortense Chatard
Robert Debré University Hospital, France
Title: Effects of age-related macular degeneration on postural sway

Biography:
Hortense Chatard has her expertise in visual neurosciences and retina. This research is integrated in her thesis work “Postural control and eye movements in AMD subjects”. The aim is to improve knowledge on the impact of AMD on postural control and to develop functional rehabilitation techniques, in order to reduce functional disability and cost of coverage.
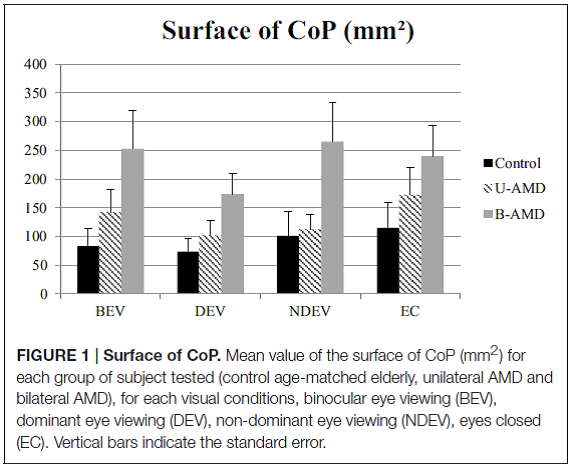
Abstract:
Age-related macular degeneration(AMD) represents a true public health issue because of the prevalence (1.6% before 64 years old and 27.9% after 85 years old), the cost of care (which increases with disease severity), psychological impact and functional disability (difficulty reading,driving restriction, etc.). According to HAS (Haute Autorité de Santé) and other authors, 33% of subjects older than 65 years have experienced at least one fall per year. It is a real public health problem because of autonomy loss and of themedical cost. Postural control iscontrolled by vestibular, proprioceptive, and visual information. The main goal of this study is to compare the impact of unilateral vs. bilateral AMDon postural sway, and the influence of different visual conditions. The hypothesis of our study was that the impact of AMD will be different between unilateral and bilateral AMD subjects compared to age-matched healthy elderly.Methods: Postural stability was measured with a platform (TechnoConcept®) in 10 elderly unilateral AMD subjects (mean age: 71.1±4.6 years), 10 elderly bilateral AMD subjects (mean age: 70.8±6.1 years), and 10 healthy age-matched control subjects (mean age: 69.8±6.3 years). Four visual conditionswere tested: both eyes viewing condition, dominant eye viewing, non-dominant eye viewing, and eyes closed. We analyzed the surface area, the length, the mean speed, the anteroposterior (AP),and mediolateraldisplacement of the center of pressure (CoP).Results: Bilateral AMD subjects had a surface area (p < 0.05) and AP displacement of the CoP (p < 0.01) higher than healthy elderly. Unilateral AMD subjects had more AP displacement of the CoP(p < 0.05) than healthy elderly.Conclusions: We suggest that ADM subjects could have poor postural adaptive mechanisms leading to increase their postural instability. Further studies will aim to improve knowledge on such issue and to develop reeducation techniques in these patients.
Faith Ukachukwu
University of Chester, United Kingdom
Title: Trachoma elimination in Yobe State, Nigeria: Will it be a “safe†way or a dead end in 2020?
Biography:
Faith Ukachukwu is an Optometrist with clinical and research interest in primary eye care, community eye health, low vision and rehabilitation. He adopts a public
health approach in exploring critical eye care issues. His published work investigated refractive error distribution in children in an urban population in Nigeria. He
combines his experience and passion to advocate for blindness prevention, actively engage in eye health education and delivers papers at conferences.
Abstract:
Trachoma accounts for 4.2% of blindness in Nigeria and 17.9% of the blindness prevalence (2.5%) in Yobe state. Trachoma prevalence in children aged 1-5 years is 35.7%. The socio-economic burden includes visual disability, decreased productivity and reduced quality of life. Trachoma has remained endemic in Yobe state, despite WHO’s recommended SAFE strategy, (which includes Surgery, Antibiotics, Facial hygiene, and Environmental sanitation), to prevent the spread of trachoma and eliminate it by 2020.
PURPOSE
This evidence review study was conducted to identify the factors militating against the elimination of Trachoma in Yobe state and the feasibility for its ‘SAFE’ end in 2020.
METHOD/FINDINGS
A review of the literature on Trachoma prevalence in Yobe state, Nigeria and implementation of the SAFE strategy was conducted to identify gaps and opportunities of public health interventions to assist in eliminating Trachoma by 2020. Although, the evidence shows substantial coverage of Azithromycin distribution in Yobe state, the enduring cycle of Trachoma transmission is likely to be caused by absence of fly vector control, overcrowded households, poor sanitation, inadequate toilet facilities, lack of clean water, poverty and social inequalities, absence of a national Trachoma policy and disruption to services due to terrorism.
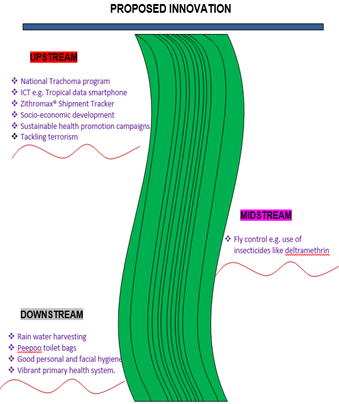
PROPOSED INNOVATION
There is a need for stronger upstream interventions, within the development of a national Trachoma program just like Ghana and Gambia. Investment in innovative Information and Communication Technology (ICT) like the Tropical data smartphone app could help monitor progress of elimination efforts, and Zithromax® Shipment Tracker could track donations of drugs to Yobe. Government should prioritise socio-economic development, sustainable health promotion campaigns and fighting terrorism. Midstream intervention includes use of deltamethrin insecticides to control flies such as has been done in Gambia. Downstream intervention involves rain water harvesting, introduction of Peepoo disposable single-use toilet bags for defecation, promotion of good personal and facial hygiene, and strengthening of primary health system.
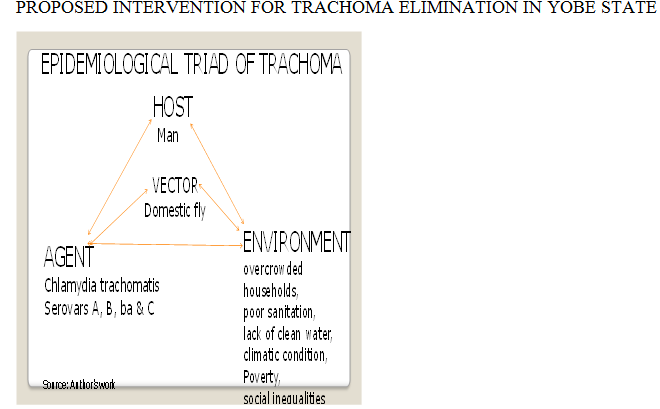
CONCLUSION
Properly implementing the F and E aspect of the SAFE strategy and the strong action across three streams of prevention identified will reduce transmission and bring us close to trachoma elimination if not in 2020 perhaps in the decade afterwards.
Erwan David
University of Nantes, France
Title: A new experimental setup to study the central and peripheral visions with gaze contingent protocol and artificial scotomas
Biography:
Erwan David is a PhD student in the LS2N laboratory (University of Nantes, France). After completing Master degrees in social and cognitive psychology (2014), then in cognitive sciences (2016) he is now studying visual attention in a multidisciplinary position, harnessing knowledge from computer science, psychology and vision science to create new visual attention models. With his team, they are studying central and peripheral visions' idiosyncracies thanks to patients with visual defects (glaucoma, AMD) and normal participants.
Abstract:
Understanding roles played by the processing of central and peripheral stimuli would mean a better understanding of the
ocular behaviour and strategies of patients with peripheral or central visual field defects. This could lead to detection tests,
visual field restoration therapies, or adapted viewing devices and applications designed to help visually-impaired individuals.
Considering this, we devised an experimental setup to simulate scotomas during visual tasks. This protocol relies on online
eyetracking data to modify on-screen stimuli; applying a mask covering part of the screen. For instance, this mask can be a
disk displayed at the center of the participant’s vision, effectively preventing any sampling of the scene with the fovea. The
eyetracking device continuously sends gaze positions to the rendering computer which modifies the display accordingly. One
issue here has to do with the delay between eye movements and relocation of the mask, for scene perception has been reported
at very low latencies. A maximum latency of 13 milliseconds was achieved by relying on the GPU acceleration to update the
scene with the latest gaze position. In our application, the rationale stemmed from the fact that experimenting on patients
presents many drawbacks (e.g. variability of visual defects, cognitive idiosyncracies of elderly subjects and evolution of coping
strategies); but this protocol allows the study of visual defects with normal participants through simulation. The nature of the
masks is binary (hiding part of a surface, showing the remainder) as in the previous example. Though, we know that visual field
defects can be experienced in many ways, this is why this protocol allows adjusting the size, deepness, form and localization
of the defect. This setup could find applications in visual field training. It might become useful in training patients toward
developing proper pseudofoveas in the case of AMD.
Nuha Fath Elrahman
Al-Neelain University, Sudan
Title: Infantile blindness: Causes and role of inheritance

Biography:
Nuha Fath Elrahman obtained PhD in Optometry and Visual Science in 2009. She started the Department of Medical and Ophthalmic Photography and is the
Head of the Department of Medical and Ophthalmic Photography at Al-Neelain University, Sudan. She is a Member of Al-Neelain University Senate and General
and Academic Secretary of Sudanese Union of Optometrists. She is a Member of the Medical and Health Professional Council and AOA, and attended many
international conferences.
Abstract:
The study is considered to be the first study in Sudan concerned with children who were born blind. It was aimed to find
out the main causes of born blindness, and the role of inheritance through their families. The study was done in Khartoum
State- Sudan. Any subject who was registered as blind since birth, his visual acuity 3/60 or less and agreed to participate in
this study was included. Permission was taken from the leader of the centers of blinds. Verbal consent was obtained before
examinations. Personal demographic data, history, visual acuity test and refraction, ocular examinations were taken. A
questionnaire was used to assess parent's relationship and history of blindness. A total number of 211 subjects were screened,
120 subjects (56.87%) were suitable. 75.83% males and 24.17% females. Their mean age was 23.15±8.1 years. The causes of
born blindness were congenital cataract (28.33%), corneal abnormalities (28.33%), optic nerve defects (27.5%) and retinal
abnormalities (5.83). Structural abnormalities (3.33%) and 6.68% of the subjects were without ocular anatomical defects. 75%
of the subjects showed positive family history of blindness, 93.33% of the subject's parents were related (71.66% of the parents
were of 1st degree cousins, 10% are 2nd degree and 11.67% far relationship). 75% of childhood blindness was inherited (51.66%
autosomal recessive, 9.17% autosomal dominant, 14.17% X-linked, 25% isolated cases).
- Innovations in Optometry | Imaging Techniques | Ophthalmic Instruments | Visual Optics
Location: Paris

Chair
Juan Bolívar Parra
DO-FIAO, Spain
Session Introduction
Rohit Sharma
Burton Hospitals NHS Foundation Trust, England
Title: 24 hour IOP monitoring –concepts & an overview including Triggerfish

Biography:
Rohit Sharma a consultant Ophthalmic surgeon working in NHS England. Received Clinical Excellence Awards from the NHS trust for his contributions & received Fight For Sight Award by the Royal College of Ophthalmologists London. Examiner for the FRCS Exams for the Royal College of Surgeons Edinburgh Represents Royal College of Ophthalmologists London for conducting Consultant interviews. Interviewer for University Medical School & doctor recruitment in the NHS. Led "Listening in Action" work in the NHS UK, is a certified Quality Service Improvement & Redesign Practitioner, completed "True Leader" workshops & is a certified Risk Assessor. Investigation officer for significant adverse events & is on the teams for service improvement & business planning.
Abstract:
Intraocular pressure (IOP) is still one of the most important modifiable risk factors for glaucoma progression. Hence naturally,
the measurement, monitoring of IOP & its lowering by various methods (surgical, medical, laser) remains the mainstay
of effective management of this potentially blinding chronic condition. Goldmann applanation tonometry remains the gold
standard but a single IOP measurement in the clinic during office hours cannot account for the diurnal variation, nocturnal
IOP profile & postural variations which have all been found to be important. Though many of these need development, the
developments are exciting. Triggerfish (Sensimed), a contact lens sensor (CLS) is an exciting & innovative device to monitor
the 24-hour IOP. Though there are some inherent assumptions and limitations of this technology, the potential, safety and
reproducibility profile is very good. I have led the successful setting up of the first triggerfish centre in NHS England along
with my team. The potential advantages as well as the limitations of this triggerfish technology & the other methods/attempts
to address this unmet of 24 hour IOP monitoring will be discussed.

Biography:
Juan Bolívar Parra received a Doctor of Osteopathy (DO) degree from the University of Granada (1997). He is a Fellow of International Academy of Orthokeratology and Control of Myopia (IAOMC) in Budapest 2015 and member of Eurok since 2012. He is a Member of the Board of Spanish Section of the IAOMC. He is a Professor of the Master's Degree course in Clinical Optometry and Advanced Optics at the University of Granada. He had conducted over 70 graduate courses, including Course in Advanced Clinical Optometry (UEM). He has participated with papers and posters in different congresses (Eurok Budapest 2015, SAO 2016, Optom 2016, Eurok Iberica Granada 2016). For 14 years, he has run his own center in Alcalá la Real-Jaén (Centro Óptico Real). His areas of specialization are advanced contactology, especially ortho-K, highlighting for being able to customize the adaptations to be successful in cases that were previously not viable.
Abstract:
In this talk, there will be an update in Ortho-K, showing the mechanisms of action of the lenses and how the hydrodynamic
forces occur between lens and cornea work. It will be shown that it does not just work by pressing on the apex. The periphery
is even more important. The changes produced after Ortho-K in the corneal epithelium will be shown through OCT images
of real cases. The risks presented by this technique will be assessed. All current applications of Ortho-K will be exposed, not
only myopia, assessing which patients can be applied at present and which refractive defects can cover, as well as where the
Dp limits are currently. Special emphasis will be placed on the control of myopia in children, comparing it with other options,
based on the scientific evidence published. Finally we will give pearls of how we can customize the adaptations in children, in
order to optimize myopia control.

Shroug M Aldaham
Complutense, Ministry of Education, Saudi Arabia
Title: Visual field changes in type 2 diabetics without retinopathy: A review

Biography:
Shroug Aldaham has recently graduated from Complutense University of Madrid (UCM),Spain with a PhD degree in Optics, Optometry and Vision. She has aBSc (Hons) inOptometry from King Saud University (KSU), Riyadh, Saudi Arabia, and a Master of Science in Vision Science from the University of Waterloo,Ontario, Canada. She has joined the Optometry department at KSU as a demonstrator (an academic position that prepares for professorship) before joining the Master program in Canada. After her masters she returned to Riyadh and later joined the PhD program at UCM. Both of her Masters and PhD studies were Saudi government-funded research grants. She has a research experience in pediatric vision screening and visual function testing in diabetics and has published in international optometric and vision research meetings. Her research interests are pediatric and diabetic visual.
Abstract:
Background: Diabetic retinopathy (DR) progression has a direct effect on vision, which by time will cause visual deterioration.
(1) Localized visual field (VF) sensitivity losses were reported in diabetics with background DR and clinically significant
macular edema.(2,3) There is little information however about VF changes in diabetics without retinopathy.
Purpose: To review VF changes in diabetics without retinopathy.
Methods: A literature review was conducted on testing VF in diabetics without retinopathy. The search criteria considered the
type of diabetes, the type of VF stimulus presented, and the instrument used.
Results: The source of variability in the VF results in diabetics depended on the difference in the instrument and/or stimulus
used, as VF changes were reported for some instruments while others did not report any change. (i.e. whether it was standard
automated perimetry, short wavelength automated [blue-yellow] perimetry, or frequency doubling [FDT] perimetry).
Differences between type 1 and type 2 diabetics were also reported. When compared to type 1 diabetics, few studies have tested
type 2 diabetics without retinopathy.


Conclusions: Care should be taken when comparing VF changes between studies related to the type of diabetes, type of
stimulus and instrument used. This presentation will further elaborate the differences between VF tests. Also, clinical VF data
for type 2 diabetics without retinopathy will be presented; aiming to see if VF testing can be used as a clinical screening tool for
type 2 diabetics before retinopathy is detected.
- Retina | Cornea | Orthokeratology and Orthoptics
Location: Paris

Chair
Rohit Sharma,
Burton NHS Foundation Trust, England
Session Introduction
Rohit Sharma
Burton Hospitals NHS Foundation Trust, England
Title: Laser and surgical management of glaucoma-A current overview

Biography:
Rohit Sharma a consultant Ophthalmic surgeon working in NHS England. Received Clinical Excellence Awards from the NHS trust for his contributions & received Fight For Sight Award by the Royal College of Ophthalmologists London. Examiner for the FRCS Exams for the Royal College of Surgeons Edinburgh Represents Royal College of Ophthalmologists London for conducting Consultant interviews. Interviewer for University Medical School & doctor recruitment in the NHS. Led "Listening in Action" work in the NHS UK, is a certified Quality Service Improvement & Redesign Practitioner, completed "True Leader" workshops & is a certified Risk Assessor. Investigation officer for significant adverse events & is on the teams for service improvement & business planning.
Abstract:
Glaucoma is a slow insidious sight threatening condition which can potentially cause irreversible visual field loss and blindness. Successful treatment is imperative after timely detection and monitoring. Current management usually starts with ocular hypotensive agents (eye drops) which need regular compliance and can have local and systemic side-effects. Laser
management includes laser trabeculoplasty (argon and selective) for open angle glaucoma, peripheral iridotomy for angle closure and iridoplasty. Cyclodiode laser is used for nonseeing eyes, intractable glaucoma and also in seeing eyes in certain conditions. Trabeculectomy filtration surgery with antimetabolites is still the gold standard invasive surgery. There are specific indications for glaucoma drainage implants like tubes. Recent advances include minimally invasive procedures like XEN, Istent which have their place in the armamentarium. An overview of the various laser and surgical options of glaucoma management for a general ophthalmologist, optometrist and general practitioner perspective shall be presented by a practicing glaucoma
surgeon.
Nuha Fath Elrahman
Al-neelain University, Sudan
Title: The impact of Rose -K RGP contact lens wear on the visual performance of keratoconic eyes

Biography:
Nuha Fath Elrahman obtained PhD in Optometry and Visual Science in 2009. She started the Department of Medical and Ophthalmic Photography and is the
Head of the Department of Medical and Ophthalmic Photography at Al-Neelain University, Sudan. She is a Member of Al-Neelain University Senate and General
and Academic Secretary of Sudanese Union of Optometrists. She is a Member of the Medical and Health Professional Council and AOA, and attended many
international conferences.
Abstract:
Aim: The study was designed to be a comparative cross sectional study. It was aimed to evaluate the effect of rigid gas permeable
contact lense wear (Rose-k menicon) on visual performance (vision, color vision and contrast sensitivity) in keratoconic
patients with different degree of keratoconus. Material and method: The history of the patients was taken to be sure that the
patient have no history systemic and ocular diseases, the corneal curvature was measured by auto refkratometer (Nidek)
to determine the degree of KC, the vision was tested by Snellen´s test type (E-test). Refraction was done subjectively using
(stenopic slit), Rosek2 lenses (menicon) was use to correct refractive sate of the eye, the color vision was evaluated with
(Ishiaraa) test and contrast sensitivity with (low contrast slip Thark), these measurements were taken with and without Rose
k2 contact lens. Results: The data were analyzed using SPSS program and the following results were obtained: A total number
of 50 patients (100 eyes) were found to fulfil the criteria of selection (31 males and 19 female) their ages were ranged from
10 - 35 years with a mean of (22.72 years ±5.79). Ninety four percent of the patients had moderate (52%) to sever (42%)
keratoconus. Their base line vision ranged (1/60-6/9) with mean of 0.10±0.10, 99% of them less than 6/18, and with rose-k 2
contact lens was from (6/12 to 6/6 ) 97% their vision was within the normal limits from (6/9 to 6/6) with a mean of 0.88±0.20,
Independent t-test showed significant differences base line and with rosek2 P value 0.000 . The base line color vision showed
that 62% of the patients showed abnormal color vision and Chi-squire test yielded a significant difference between base line
color vision and color vision with contact rose -K CL P value 0.016. The base line contrast sensitivity ranged from 0.5 to 125
with mean of 1.08±0.14. 62% of the patients showed abnormal base line contrast sensitivity compared to 100% of normal
contrast sensitivity with rosek2 mean 1.25±0.00. Paired sample t-test showed a significant difference between baseline contrast
sensitivity and after wearing rose K contact lens P 0.000.
Conclusions: Rose -K RGP contact lenses significantly improve the visual performance













